There’s no doubt that we live in an age of change. 2016 registered seismic shifts in politics, culture and finance that, whether they exhilarate or frighten us, will shake the ground under our feet for years to come.
So it’s reassuring to start 2017 by looking back at some of the impressive changes in medical technology that the western suburbs gained in 2016. Whether they save lives — like the "strokemobile" that delivers crisis care to patients’ doorsteps — or save hairlines — like using platelet-enriched plasma to reverse baldness — these advances can’t help but give change a good name.
Mobile Stroke Unit Hits the Road
Time is critical when rushing a stroke patient to the emergency room. Every minute an ambulance driver spends crawling around traffic jams or waiting out freight trains can cost his patient nearly 2 million neurons, while testing at the hospital eats up another 10 to 20 minutes. That much delay can lower the patient’s recovery chances by 12 percent and take more than two years off his life, says Dr. Harish Shownkeen, an interventional neuroradiologist at Northwestern Central DuPage Hospital in Winfield.
That’s why Shownkeen and his colleagues launched a project to build the first mobile stroke unit licensed in Illinois, which is also just the sixth licensed in the U.S. The unit and its staff were scheduled to start test runs in late December and go into service in early January.
"This is a quantum leap in stroke treatment," Shownkeen asserts. "We’re bringing the hospital to the patient."
The oversized ambulance lets specially trained paramedics begin diagnosis and treatment as soon as the patient is inside. It contains a 16-slice CT scanner that produces images of the patient’s brain within 10 minutes, along with blood test analyzing equipment that returns results in less than a minute. All scan and test results are automatically transmitted wirelessly to ER physicians.
Once the stroke is confirmed and its type — ischemic or hemorrhagic — identified, the paramedics can start an intravenous infusion of either clot-dissolving drugs or clot-promoting drugs to re-establish blood flow to the brain. Best of all, when the mobile stroke unit (MSU) reaches the hospital, the patient can be whisked into a prepared operating room for immediate surgery instead of having to go through testing and diagnosis in the ER.
"Three years ago we could never have fathomed that we could treat stroke patients 15 minutes after we get the 911 call," commented Showkeen. "Normally it takes at least that long just to get patients into the ER."
When calls come in from CDH’s response area — Carol Stream, Glen Ellyn, Warrenville, West Chicago, Wheaton and Winfield — dispatchers will send the MSU and a standard ambulance team to any call reporting a suspected stroke. If the ambulance team arrives first, it will stabilize the patient until the stroke unit arrives unless it’s obvious that the patient is not suffering a stroke, in which case paramedics will handle the call as usual. If the MSU arrives first, it’s stocked with all the supplies and equipment that a standard ambulance carries so that its team can take care of non-stroke patients until the standard ambulance arrives.
Either way, CDH and Northwestern Medicine, its parent company, will donate all MSU services for the foreseeable future, according to Shownkeen. "This unique service is what we’re giving back to the community. Maybe in five or 10 years MSUs will be common, and then we’ll start charging for it," he said. "But now it’s too important for stroke victims not to make it available without impediment."
Giving Pain the Cold Shoulder
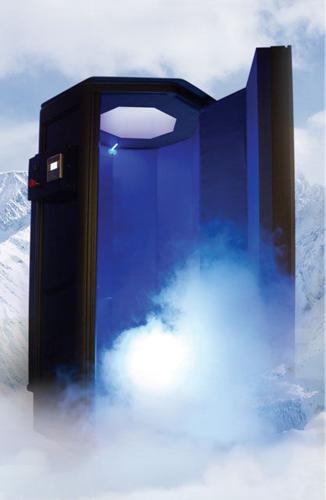
Cryotherapy — applying extreme cold to body tissues for medicinal purposes — has been used for years in cosmetic procedures like facials and "cool sculpting" to freeze off unwanted fat. Now several area clinics are using the same technology to provide relief from arthritis, fibromyalgia and chronic back pain, among other conditions in which inflamed neurons flood the brain with extraneous pain signals.
"In 1969, a study at the University of Tokyo examined using cryotherapy to treat rheumatoid arthritis by stimulating the body’s healing response," explains Dr. Jessie Cheung, who owns DuPage Dermatology and Laser Center in Willowbrook. "Back then the technology to apply cold wasn’t advanced enough to be truly effective. The new technology we have now has the capability we need to really help people."
Cheung uses a small cryotherapy chamber, reminiscent of an old-fashioned sweat bath, to bombard her patient’s underwear-clad body with nitrogen vapor that’s -250 degrees Fahrenheit. The three-minute-long dry treatment reduces the skin’s surface temperature to about 40 degrees. Since the patient’s head sticks out the top of the chamber, the patient breathes normal room air during the procedure. "It’s cold, especially in the last 30 seconds, but it’s not painful and the skin isn’t frostbitten," says Cheung.
This drastic cooling of the epidermis prompts the circulatory system to constrict surface blood vessels to preserve core body heat. When the treatment ends and the patient leaves the chamber, the body quickly expands those blood vessels, flooding the surrounding muscle and nerve tissue with warm blood enhanced by endorphins and the neurotransmitter cytokine. Since cytokine levels are often unbalanced in people with chronic nerve pain, the overload restores the balance and calms the symptoms for days or, sometimes, weeks.
A 2013 study released by the National Institutes for Health confirms that cryotherapy relieves symptoms and improves the quality of life for fibromyalgia patients. "We speculate that this improvement is due to the known direct effect of cryotherapy on the balance between pro- and anti-inflammatory mediators having a recognized role in the modulation of pain," according to the NIH abstract of the report.
Cheung says that most of her cryotherapy patients start with two or three treatments per week, then taper down to once a week within a month. While the treatments — which range in cost from $25 to $65 per session — aren’t covered by most insurance carriers, they often allow patients to reduce the amount of pain medication they take, which lowers their pharmacy bills, she adds.
GoPolar Cryotherapy in Lemont and French MedSpa in St. Charles and Elgin also offer whole-body cryotherapy services.
Gone today, Hair Tomorrow
For years orthopedic specialists have used platelet-rich plasma injections to speed healing of sprains, tears and other joint-related injuries. Who knew the same procedure could also regrow hair?
Cheung says she got the idea to try injecting PRP into patients’ scalps after hearing about experiments in surgically wounding the scalp to prompt the body’s immune system to reactivate dormant follicles as part of the healing process.
"Turning deactivated hair follicles back on is all about the cell messengers — chemicals that transmit messages between cells in the body," explains Cheung. "Platelets contain epidermal growth factors as well as cytokines and other growth-related messengers, so infusing plasma with extra platelets and injecting that into the scalp should be more effective than just drawing blood to that area."
Laboratories create PRP by collecting some of the patient’s blood and centrifuging it several times to isolate the plasma and platelets from the other blood components. The resulting semi-solid tissue contains about five times as many platelets per ounce as whole blood does. Cheung says that she extracts about 20 milliliters of blood for each treatment.
Most patients start noticing new hair growth about two weeks into the treatment process, with substantial growth after six weeks, Cheung reports. While each treatment cycle can vary in length and cost, the average cycle costs about $1,200. Most patients — especially younger ones — need just one cycle of treatment to start hair growth and keep it growing, she adds.
"It’s not cheap, and insurance companies don’t cover it," acknowledges Cheung. "But a hair transplant starts at $50,000 and it’s much more invasive than PRP injections. My patients usually say that the results are well worth the money."
An Outside View of Coronary Artery Disease
At most hospitals, undergoing an angiogram to discover possible blockages in coronary arteries involves lying still, often under sedation, for one to three hours while a doctor threads a sensor-tipped wire through the blood vessels to measure and compare blood pressure readings before and behind potential blockage sites. The patient can’t eat or drink for at least four hours before the procedure; must go without blood thinners for three days beforehand and one day afterward; and usually needs a day of rest to recover from the procedure. Worse, occasionally the catheter snags plaque deposits on its way through the blood vessels, pulling them free and leaving them in the bloodstream to potentially create a new blockage.
At Loyola University Medical Center in Maywood, many angiogram candidates can choose instead to have their coronary arteries mapped by a high-resolution 256-slice CT scanner, with no preparation beforehand, no recovery time, and nothing at all inserted into their bodies. Called a fractional flow reserve CT scan, the procedure takes only a few minutes and provides doctors with a comprehensive three-dimensional image of the arteries that includes any clots, narrow spots or other blockages inside them.
"Patients love it," asserts cardiologist Dr. Mark Rabbat, an assistant professor at Loyola’s Stritch School of Medicine who educated colleagues about the new test at last November’s American Heart Association scientific conference. "Instead of spending hours at the hospital, they’re in and out in minutes. The scan itself takes about 10 seconds, and then they’re free to get back to their lives."
Once the patient has been scanned, a 3D mapping computer melds the 256 planar images into a virtual model that shows a snapshot of the patient’s blood flow during the scan. "We use standard models of fluid dynamics to simulate the patient’s blood flow under stress," Rabbat explains. "It’s fantastic because it’s really accurate. In fact, we’ve been able to pick up a lot of (coronary artery) disease that we’d been missing with angiograms, and we’ve been able to safely defer surgery for patients whose coronary artery disease is less serious."
Patients who do need angioplasties or other catheter-driven procedures have more successful surgeries because of the 3D scans, Rabbat adds. "This technology allows us to use the catheter lab more efficiently because it gives us extra detail to work with," he explains.
The FFR-CT test won Food and Drug Administration approval in August 2015. So far, Loyola is the only west suburban hospital to adopt it, according to Rabbat. "I expect we’ll see it at other hospitals here and around the country in the near future," he says. "It has the potential to completely revolutionize the way we approach cardiac care."
The Arterial Stent that Removes Itself
For decades, cardiologists have fixed weakened arteries by inserting stents — small, solid or mesh metal tubes that hold the artery walls apart so the artery stays open. Once a stent is implanted, it stays with its owner until death does them part.
While that’s not a problem for most people, a few cardiac patients have experienced scarring inside their arteries because the ends of their stents scratched the arterial wall. Other patients with chronic arterial issues end up with multiple stents in the same artery that hold it rigid for inches at a stretch, states Dr. Patrick Fenner, a cardiologist at Advocate Good Samaritan Hospital in Downers Grove.
"Every stent in somebody’s artery becomes an added layer inside that artery, making it narrower than it originally was," Fenner points out. "Another long-term problem is that, if you put a metal scaffold into a blood vessel, from then on that blood vessel can only be the same size as the stent. Normally, blood vessels expand and contract depending on changes in blood flow and pressure, which helps regulate those functions throughout the body. Having stents in permanently keeps those arteries from fluctuating."
The Absorb stent, designed by Abbott Laboratory, doesn’t cause those problems because it’s bioresorbable, Fenner says. The device, which gained FDA approval last March, is made of crystallized polylactic acid that starts to dissolve months after insertion and completely disappears in about three years. It’s already being used in 100 countries, according to Diagnostic and Interventional Cardiology Magazine.
"We’ve been waiting a very long time for this technology. I hope it lives up to its promise," states Dr. John Lopez, an interventional cardiologist at Loyola University Medical Center. "It’s the first step in a real shift in how we treat arterial disease."
While the Absorb stent has been proven safe and reliable, Lopez says he’s not sure it improves patient outcomes in the short term. "What we need is more patients with longer follow-up times. That will give room for us to learn more about how the stent interacts with the patient."
Knowledge gained from the Absorb stent could help researchers create more interactive stents that provide varying levels of artery wall support during their lifetimes, both doctors agreed. "Ten years from now we will look back and say that this device is primitive," predicts Lopez.
Look, Ma — No Leads!
In 1926, the first working model of a pacemaker used a large generator attached to a needle that was plunged through the patient’s chest wall into the heart. By the early 1950s, surgeons were able to implant leads into the heart that stuck out through the skin and connected to a 5-lb. 12-volt battery that the patient could wheel around on a cart, which at least enabled users to leave their rooms once in awhile. The 1958 success of the first pacemaker battery small enough to be implanted just under the patient’s skin made headlines around the world, even though the advance required a surgically-created flesh pocket inside the chest connected to the heart by leads strung through major cardiac veins, which created a host of related medical issues.
Almost 60 years later, the next leap forward for pacemakers won approval this past April. The Micra pacemaker combines both leads and battery into a capsule not much larger than a multivitamin tablet. Instead of cutting into the chest to implant it, a cardiologist simply attaches the Micra to a catheter that he then guides through the veins into the right ventricle. Once there, a spring releases the pacemaker and spreads four tiny, flexible tines that latch onto the ventricle wall. Contact with the muscle tissue is all the Micra needs to read the heart’s beat pattern and administer electrical pulses to correct it as needed.
"Eventually all pacemakers will be built like this," predicts Dr. Ken Weinberg, an interventional cardiologist with DuPage Medical Group, adding that the Micra is only a single-chamber pacemaker that can’t replace a traditional dual-chamber pacemaker. "The benefits to a leadless pacemaker that sits directly inside the heart are enormous."
To start with, the subcutaneous pocket for a traditional pacemaker generator is easily damaged and prone to infections, particularly during the first few months after implantation, Weinberg says. Surgeons also have to cut into the chest to reopen the pocket every time the generator malfunctions or its battery runs out, which also promotes infections.
The leads that connect the generator to the heart also can injure the patient from the inside. "You have 60-centimeter (two-foot-long) electrical wires permanently going through the subclavian vein that are not supposed to be there," Weinberg notes. "Blood clots can form around the leads, which can cause blockages or infections. Leads often have to pass near ribs or the clavicle, and if they rub against the bones they can wear away the insulation."
The Micra pacemaker avoids these issues by incorporating very short leads into the generator and putting the whole thing inside the heart. While removing the device is more difficult than implanting it, Weinberg maintains its lack of moving parts and its 10-year-rated lithium hybrid silver vanadium battery make it far less likely to need removal than a traditional pacemaker. Tests also have shown that if the heart muscle grows around the Micra, it can be remotely turned off and remain safely in place while a new unit takes over.
This new pacemaker design will improve rapidly in the next several years, Weinberg asserts. "This is version 1.0. While Medtronic is the first to bring it to market, there are a lot of companies working on this technology. The next versions will be smaller and more interactive with other devices," he says. "One company is working on a leadless pacemaker that will electronically ‘talk’ with an automatic defibrillator (if the patient goes into ventricle fibrillation) to stabilize the heartbeat. Probably we’ll see two-pacemaker systems that have one in the ventricle and another in the atrium that communicate to manage the heart rhythm."



(0) comments
Welcome to the discussion.
Log In
Keep it Clean. Please avoid obscene, vulgar, lewd, racist or sexually-oriented language.
PLEASE TURN OFF YOUR CAPS LOCK.
Don't Threaten. Threats of harming another person will not be tolerated.
Be Truthful. Don't knowingly lie about anyone or anything.
Be Nice. No racism, sexism or any sort of -ism that is degrading to another person.
Be Proactive. Use the 'Report' link on each comment to let us know of abusive posts.
Share with Us. We'd love to hear eyewitness accounts, the history behind an article.